Diabetes mellitus is a chronic metabolic disease, yet it has established psychological relations and consequences. This article describes findings with respect to the psychological aspects of diabetes in adults and adolescents. Also, explore how psychological interventions help in coping with diabetes.
Relationship of psychological stress with diabetes
The connection between diabetes and psychology has been established in various research studies. Several clinical trials have demonstrated that emotional stress in diabetics is linked to poor glycaemic control, a deficit in self-care behavior, and adverse diabetes outcomes. A research study by Gonzalez et al. demonstrated the relationship between depression and poor adherence to medical treatment and diabetes self-care after nine months. Similarly, another research revealed that persistent depression was due to poor self-management in terms of diet and exercise over a subsequent period of five years. However, a reduction in depressive symptoms was found to be associated with improved blood sugar control.
Furthermore, evidence from research studies shows that psychological factors may contribute to gastrointestinal, metabolic, and sexual dysfunction in diabetics. Research by Lustman et al. investigated the connection between diabetes symptoms and depression and identified that diabetes symptoms are more likely to be related to depression than glucose control. Moreover, a combined study by Clouse and Lustman evaluated that psychiatric issues such as anxiety disorder and depression were significantly linked with sexual problems. Hence, this evidence from research studies establishes that psychological factors greatly affect diabetes outcomes.
Emotional distress in diabetics
The patient’s perception about their health condition will affect the way how they cope with the condition. Considering that living with diabetes is a lifelong process and requires proper management of psychological problems, the psychological reactions of diabetics are divided here into four basic levels of emotional distress.
-
- Emotional reactions
- Shock
- Denial
- Guilt
- Anger
- Anxiety
- Diabetes distress
- Confusion regarding self-management
- Trouble communicating
- Distress in picking among different foods in the family
- Phobia reactions
- Fear of starting on insulin injections
- Hypoglycaemia (low blood sugar)
- Complications
- Obsessive behavior
- Psychiatric disorders
- Anxiety
- Depression
- Eating disorder
- Delirium (confusion, disorientation, and trouble concentrating)
- Schizophrenia
- Bipolar disorder
Eating disorders can affect glycemic control and increase the risk of diabetes-associated complications. In a study, it has been revealed that patients with night eating syndrome are likely to be obese and depressed, have poor sugar control, and are associated with a high risk of diabetes complications.
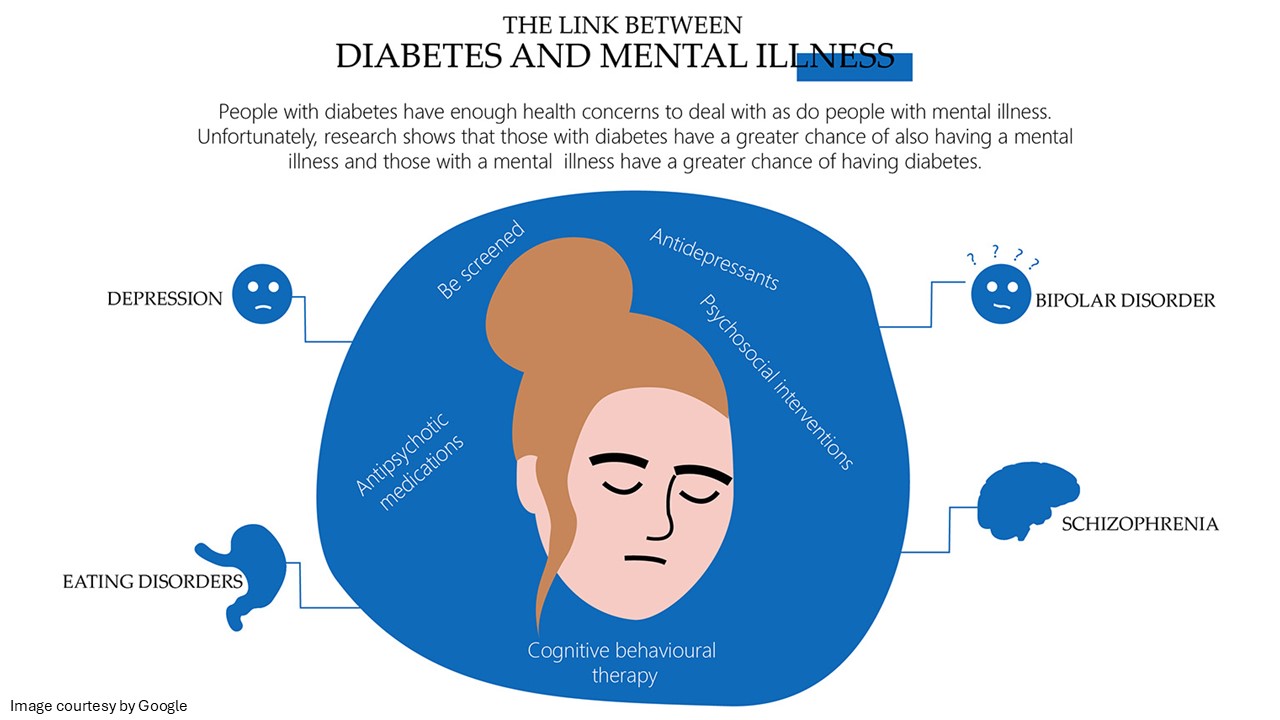
Depression could cause obesity and diabetes through lifestyle factors, including a sedentary lifestyle, overeating, and poor self-care. Also, diabetes diabetes could be associated with depression because of major emotional, financial, and medical burdens incorporated into diabetes management. Additionally, the use of anti-depressants increases body weight and contributes to insulin resistance and, thereby, Type 2 diabetes. Research shows a close bond between diabetes and schizophrenia.
Psychological strategies & counseling
Diabetes psychological effects have brought a greater focus on psychological interventions. Effective diabetes management requires continual, complex, and demanding self-care behavior. It is well known that psychological stress is a common problem in people with diabetes. Considering the importance of psychological factors in diabetes management, there is a need to implement effective interventions for diabetes support in people dealing with the daily challenges of life.
Psychological coping strategies for diabetes include motivational therapy, cognitive behavioral therapy, coping skills training, problem-solving therapy, and family behavioral therapy, which have been shown to enhance treatment adherence and attain the goal of glycemic control. These psychological strategies have been identified as an important part of the diabetes management plan.
These interventions target depressive symptoms, glycaemic control, diabetes-specific distress, interpersonal functioning, and anxiety adherence to medication regimen. Moreover, these strategies are extremely effective at improving blood sugar levels and self-care behavior (dietary recommendations, physical exercise, and self-monitoring of blood glucose levels), thus lowering the risk of diabetes-associated complications and improving the overall quality of life.
Cognitive behavioral therapy consists of a single session in the beginning to improve adherence to medical treatment and self-care behaviors. The latter part of the therapy consists of 9 to 11 sessions that target adherence and depression. These sessions carry motivational interviewing and typical techniques like behavioral activation, monitoring of glucose levels, mood, and dietary and physical activities. Motivational interviewing is considered an independent counseling approach that builds motivation for dealing with diabetes-associated challenges. It is an extremely effective strategy for supporting people with diabetes in overcoming resistance.
Complementary therapeutic techniques, including yoga, are also an effective approach for the care and management of type 2 diabetes. Practicing yoga not only improves the symptoms but also has beneficial effects on multiple other body functions that are adversely affected by diabetes. Yoga has been shown to cause a significant improvement in blood sugar control, fasting blood glucose levels, postprandial blood glucose, HbA1c, lipid levels, and body composition. Furthermore, yoga practice has been found to be associated with a reduction in body mass index, depression, anxiety, improved cognitive function, oxidative stress, and general well-being.
Summary
Patients who have diabetes have an increased risk of developing common mental health issues, including anxiety and depression. A large number of patients experience diabetes distress in response to disease burden and associated threats. Diabetes patients experience cognitive dysfunction that may range from mild to very severe. In addition, the condition may cause a significant reduction in the patient’s overall quality of life. Psychological factors, including anxiety and depression, can cause complications in managing diabetes, yet most people do not have access to a psychologist.
In most cases, psychological issues associated with diabetes can be lessened with the help of a psychologist. Along with medical management, psychological strategies and counseling are introduced into the diabetes management plan to deal with mental health issues, poor quality of life, problems with self-management, and adherence to medical treatments. Core psychological interventions such as cognitive behavioral therapy, motivational interviewing, yoga, and counseling strategies have proven to be effective in achieving good glycaemic control and reducing depression.



