Posted July 7, 2014
2302
0
0
The American Cancer Society recommends women to start mammography screenings at the age of 40. Additionally, it recommends that women at higher risk of breast cancer (with a cancerous family history), should go for regular breast MRIs, if a mammogram screening shows any abnormalities.
However, recent guidelines by the U.S. Preventative Services Task Force suggest that mammography should advisably start at the age of 50 instead of 40, however this is only a suggestion for the average woman. What should women with average or high risk of breast cancer do? We take a close look.
General Guidelines and Age Recommendation
According to the U.S. Preventative Services Task Force, screening mammograms is recommended for women. The recommendation applies to the average woman. Women at very high risk should go for mammograms at the age of 40 or start even sooner. A mammogram is necessary at any age in the event of a lump being found in the breast.
Basically, regular mammograms are a good step to detect breast cancer early on, thereby leading to more chances of survival upon early treatment.
There are several factors that decide what age a woman should start mammograms.
Women who are not at high risk of breast cancer can start mammogram screenings at 50. However, just to be on the safe side, it is advisable for a woman to go for one mammogram at the age of 40 to 45; if it turns out normal, the next mammogram can happen at 50. The National Research Center for Women & Families and their Cancer
Prevention and Treatment Fund has been advising this standard for a couple of years now.
For those who are at high risk of breast cancer, mammograms should begin at an earlier age. The age of 50 is a standard guideline for the average woman who is not at high risk and shows no symptoms. However, if a woman detects a lump, a mammogram should happen right away, irrespective of her age. Also, in general, a woman who is at higher risk of breast cancer—owing to various reasons such as environment exposures or family history of cancer—should go for regular mammograms after the age of 40, or even earlier, to be cautious.
If a woman has been tested positive for the BRCA genetic mutation, she is at higher risk of developing breast cancer. Earlier, annual mammograms between 25 to 35 were recommended for carrier of this genetic mutation. However, recent studies have something else to say. It is now said that mammograms before 35 are futile, and in fact, harmful. This is due to the increased exposure to radiation during mammograms, which shoots up the risk of developing breast cancer induced by radiation. In short, it is possible that a woman might not have developed breast cancer otherwise, but ends up getting it as a result of starting mammograms too early and being exposed to higher radiation in her lifetime.
Any woman who has a close relative such as a mother, grandmother or a sister with a history of breast cancer when they were 50 or older has a high risk of getting breast cancer. Some women can also be at high risk due to obesity. Such women are advised to go for mammograms every year or every 2 years after the age of 40.
What should young women with risk of breast cancer do? 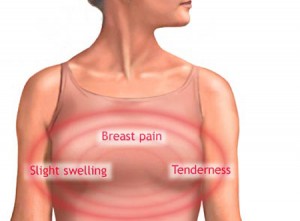
For a woman who has a close relative who got breast cancer at a younger age, regular
mammograms are advised starting before 40. The downside here is that young women have a tendency for dense breasts, which come up white on mammograms. The problem here is that cancer comes up looking white as well, thereby making mammograms pretty pointless for screening and diagnosing young women, or any woman who has dense breasts. For such women, a better and far more accurate option is a breast MRI. It is not only more precise but also safer than a mammogram.
It is worth noting that breast MRIs are more beneficial but come at a price. MRIs are much pricier than mammograms. A breast MRI costs nearly $2,000 on an average, which is a whopping 20 times more than the cost of a mammogram. Another sad news is that insurance doesn’t necessarily cover the cost of a breast MRI, unless a doctor specifically recommends an MRI owing to high risk of cancer. There is a long way to go for medical science in terms of coming up with firm conclusions on breast MRIs.
Related article: Diet and PMS: How Are They Related
Mammography according to cancer risks
Biennial mammography, which means mammography screening every 2 years, is very beneficial for all women in the age bracket of 40 to 79 who have dense breasts or a combination of family history of breast cancer and breast biopsy. This is the recommendation mentioned in Dr. John Schousboe 2011’s publication titled ‘Annals of Internal Medicine’.
Furthermore, biennial mammography is also good for women with average breast density in the age bracket of 50 to 69, as well as women with low breast density falling in the age bracket of 60 to 79.
Dr. John Schousboe is in tune with the guidelines set by the Task Force that recommends that the average woman should go for biennial screening starting at the age of 50 where as a woman who has a high risk of breast cancer should start screening before hitting 50.
At last, the age and frequency of mammography screening depends on factors such as breast density, age, family history of breast cancer, breast biopsy history as well as a woman’s personal views on the risks and benefits of mammography screening.
As a woman grows older, the risk of breast cancer escalates. The chances of getting
breast cancer are much higher after the age of 50 than when a woman is younger. Hence, as a general conclusion, annual mammograms are most beneficial for women after the age of 50. There are also most cost effective at this age. As mentioned before, mammograms started at an earlier age tend to have less accuracy and lead to unnecessary breast biopsies and needless to mention, anxiety in women.
Are more frequent mammograms better?
A lot of women think that more frequent mammogram screenings are better if they can afford it. However, it is wise to stick to standard guidelines as discussed above. Women need to remember that more mammograms mean more exposure to radiation, which in turn increases the chance of getting breast cancer.
In order to cut back exposure to radiation, it is advised that the average woman should start mammograms at 50. Less frequent mammography also equates to fewer false alarms, thereby reducing the hassle of unnecessary test, biopsies and anxiety.
Do mammograms save lives?
Regular mammograms definitely help save lives by diagnosing breast cancer at an early
stage. The number of deaths caused due to breast cancer has seen a drastic reduction in
over the years due to regular mammography. As mammography has gained popularity in recent years, a rising number of women have been diagnosed at an early stage, and the advent of new cancer treatments has saved a lot of lives. However, we have a long way to go as far as saving lives is concerned.
Stopping self-exams of breasts
According to the Task Force, breast self-exams are more risky than beneficial. Self-exams can often lead to unnecessary false alarms. In any case, by the time the cancer is evident enough to be detected in a breast self-exam, it will be found anyway. The same logic applies for doctors conducting self-exams. In short, breast self-examinations of any sort are may send false-positive or true-negative results in cancer detection and thus not
recommended.
If you have any query or suggestions, feel free to share your views in the comments box below.
Share this article if you are a woman or you care about one.